Mercedes Vega hasn’t been allowed to hug her brother, Manny, since last year.
He lives at Hollywood Presbyterian Medical Center, a hospital that also provides long-term nursing care. He has a tracheostomy so he can’t speak, but Vega knows he recognizes her, and she sees him perk up whenever she visits.
Before the pandemic, Vega saw her brother all the time. She’d watch movies with him, they’d use the community room for birthday celebrations, and she provided countless hours of unpaid care, like brushing his teeth, cleaning him, and doing physical therapy.
But ever since the Omicron variant caused COVID cases to spike, Hollywood Presbyterian Medical Center put a temporary pause on those up-close and personal visits. Now if Vega wants to see her brother in-person, it’s through plexiglass, with walkie-talkies.
“It seems like when you visit someone in prison,” she says. “There's that big window, and then there's huge distance.”
Vega has had a tough time meeting all the guidelines just to get to a plexiglass-mediated visit. Most days it doesn’t feel worth it, so instead they see each other on 15-minute meetings over Zoom, whenever the hospital’s Wi-Fi is working and the camera is positioned correctly.
To get to the plexiglass — or any kind of in-person visit at a long-term care facility in California — visitors need to show proof of a negative COVID test. It either needs to be a rapid test from the past 24 hours, or a PCR test taken in the past 48 hours.
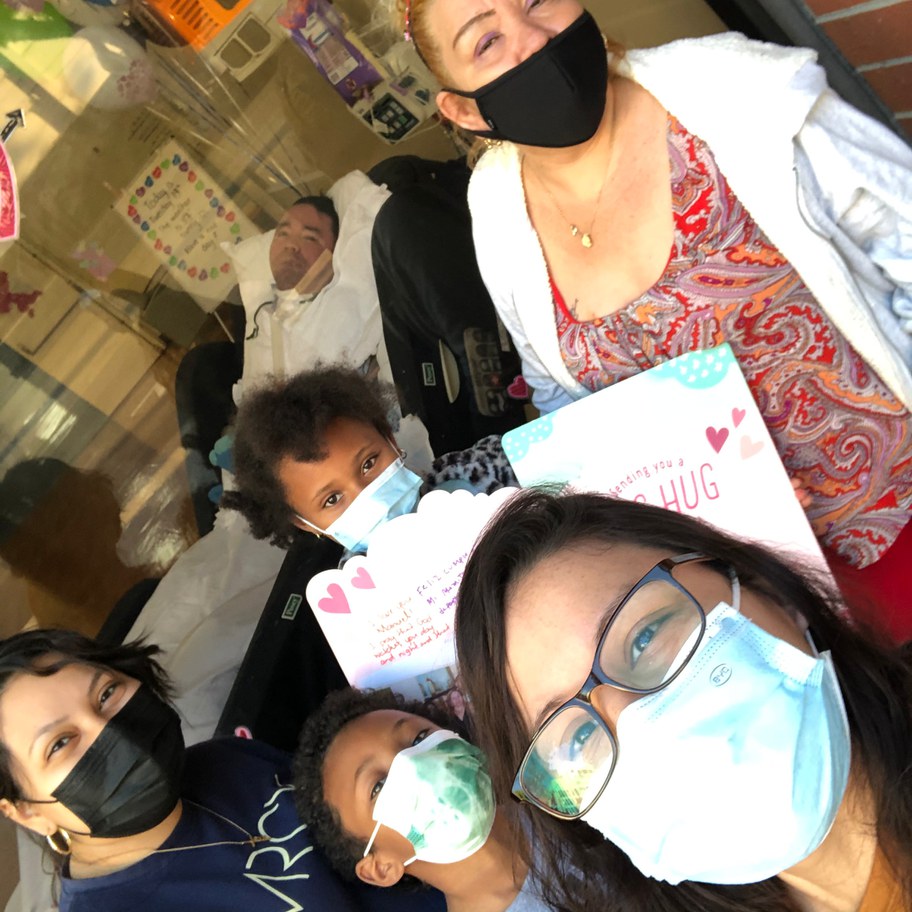
For Mercedes Vega, in-person visits look like this: approximately 20 minutes with her brother behind glass while the family stands outside. Photo courtesy of Mercedes Vega.
Sonia Anastacio says before the pandemic, she visited her husband every day since he suffered a severe stroke nearly six years ago. Now she’s having a hard time getting back in to see him at Fountain View Subacute and Nursing Center in East Hollywood, where he lives.
“Home tests are very hard to come by. I mean, everybody's pretty much out of them,” she says. “Even if we get an appointment, just getting the results back … they give us 48 hours for a PCR test. And sometimes we're getting it back within maybe 48 to 72 hours, which is senseless.”
In a statement, Fountain View Subacute and Nursing Center told KCRW they are following California Department of Public Health's regulations with their policy.
Meanwhile, as Anastacio struggles to prove it’s safe to let her inside, COVID-positive nurses in California who aren’t showing symptoms are allowed to keep showing up to work.
That’s because as of January 8, the state of California started allowing nurses, including those who work with vulnerable nursing home residents, to report for duty if they are asymptomatic — a change hospital administrators insist is necessary to keep hospital staffing at a critical level.
Governor Gavin Newsom defended the change at a recent press conference: “It’s called dealing with reality. … [It’s] what you need to do in a time of challenge, and constraints, and scarcity.”
“I strongly believe that it’s so wrong,” says Anastacio. “They go out. They're doing exactly the same thing as I'm doing. Why are they making us get tested every single time?”
Tony Chicotel, an attorney with California Advocates for Nursing Home Reform, agrees. “We have this alarming situation where COVID-positive staff can just walk right into a facility and provide care to our most vulnerable residents. Whereas a vaccinated boosted visitor who also provides critical care is completely locked out. It doesn't make any sense,” says Chicotel.
And while vigorous testing protocols for visitors might protect residents from a potentially deadly virus, it exposes them to another risk that can also have deadly consequences: long-term isolation.
Loneliness doesn’t get listed on a death certificate, of course. But a survey from public health nonprofit Altarum found that three-quarters of the nursing home residents they surveyed were lonelier in 2020 than before the pandemic. And a group of researchers with the aging advocacy group CJE SeniorLife found two-thirds of the residents they surveyed lost weight in the first year of the pandemic.
“Through experience, I find that weight is often a proxy for health. And when the weight starts to slip, the health starts to deteriorate, deteriorate, and people get sick and die,” Chicotel says. “Visitors provide connection to the outside world and engagement with the community, psychological uplift, help people avoid depression, all those things.””
Vega says her brother has lost weight, and she’s seen his dental hygiene get worse. Hollywood Presbyterian told KCRW in a statement that patient care has not been impacted by the pandemic.
Fountain View wouldn’t comment about Anastacio’s husband, citing privacy concerns. But she says he isn’t the same. “I did his grooming every day, oral care every day. They didn't have to do any of that. I did physical therapy for him, range of motion every day,” she says. “Now he's a little stiffer. … It's detrimental. My husband has deteriorated a lot.”
